As Bengaluru continues to record over 25,000 COVID cases per day, how well is the city prepared to deal with the third wave? Does the city have enough hospital beds? Is BBMP able to track and support patients in home isolation? Here’s a roundup.
In the current wave, a smaller percentage of patients seem to need hospitalisation compared to the second wave last year. However, BBMP Chief Commissioner Gaurav Gupta has emphasised that the rising case count can increase the absolute numbers of people who require hospitalisation, which can lead to a shortage of beds. A BBMP press release on January 18th said that case numbers have been increasing by 250% week-on-week.
Testing and Contact tracing
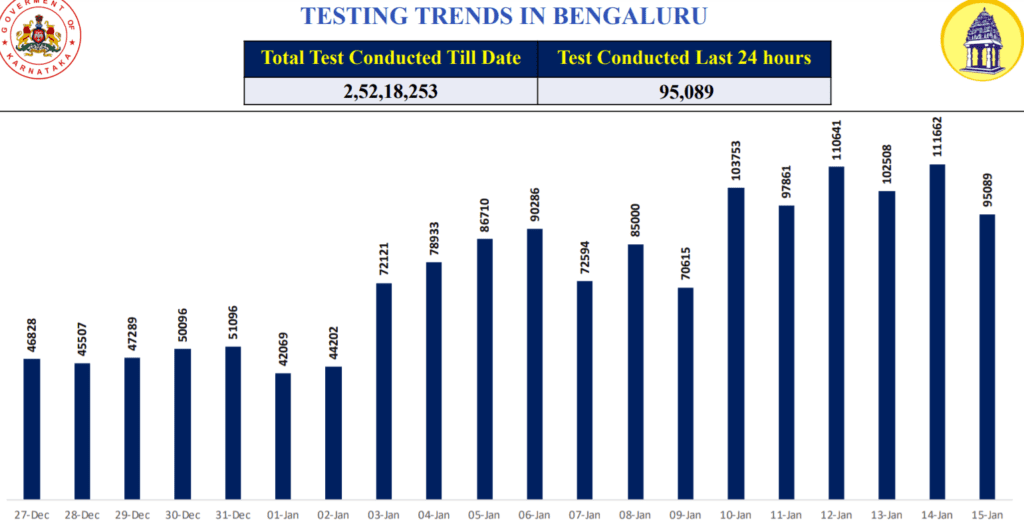
Compared to December and earlier months, the number of tests per day in the city have seen a sudden jump in January. As per ICMR’s recent guidelines, asymptomatic primary contacts don’t have to be tested unless they are in the high-risk category. The BBMP, however, has been testing primary and secondary contacts. According to BBMP press release of January 18, around 1.1 lakh tests are being done per day now.
However, Dr Bhaskar Rajakumar, Nodal Officer heading the COVID war room, says BBMP is focusing on targeted testing: “Some level of random testing will continue since groups like travellers have to be tested, but the majority is targeted testing,” says Dr Bhaskar. “Approximately 10-20% of tests are done on symptomatic people. And the rest is done in containment zones, among the primary and secondary contacts of patients, and among high-risk population such as pregnant women and those with comorbidities.” (The total daily count includes people whom BBMP tests and those who approach private labs for tests.)
As of January 17th, the city had 627 containment zones, the majority of which are in apartments.
Read more: “Cities need more decision-making powers to fight COVID-19”
Dr Bhaskar says testing of contacts is only advised and is not mandatory. As per BBMP’s advisory to apartment associations/societies issued on January 13th, testing is mandatory for those who are symptomatic. “Ideally, even those without symptoms should undergo testing so that they don’t inadvertently spread the virus, but we are not forcing them to get tested. It’s up to the citizen to be a good Samaritan and get tested”.
For primary contacts, testing is recommended on the fifth day of quarantine, considering the incubation period of the virus. And those who use self-test kits are supposed to upload their results on the company’s app.
Helplines and triaging
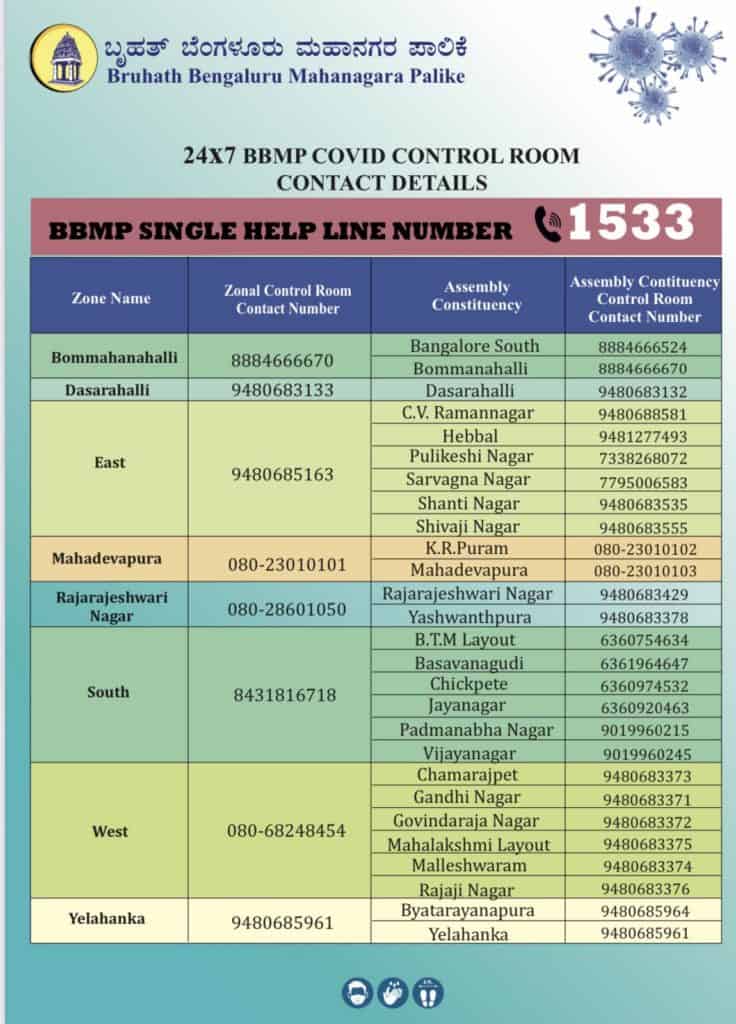
Currently, BBMP has a central helpline (1533), a zonal helpline for each of the eight zones, and a separate set of helplines for each of the 27 assembly constituencies in the city.
When a person tests COVID-positive, an executive from the relevant zonal/constituency-level control room will call them and do tele-triaging to assess their condition. Across all zonal control rooms, around 20,000 such calls are made daily at present, according to Dr Bhaskar. Of these, around 20% (3,000-4,000 cases) would require physical triaging due to the patient’s condition or because they fall in the high-risk category.
Physical triaging is done through Mobile Triaging Units (MTUs, which include a doctor and a team) that visit the patient at their home. Based on the patient’s condition and facilities available at home, the team may recommend either home isolation or shifting to a hospital/COVID Care Centre.
As of January 17th, BBMP had 318 MTUs. “While all 198 wards have at least one, some have 3-4 MTUs,” says Dr Bhaskar. (The Palike also has physical triage centres where patients can walk in.) Asked whether the MTU system would be scaled up to cover more patients, Dr Bhaskar said “It’s humanly impossible to physically triage 20,000 cases a day. For that you need 2,000 doctors on the field. One doctor can triage a maximum of 10 cases a day, and that itself is a stretch.”
While the current manpower of MTUs seems sufficient to deal with the present caseload, numbers are increasing rapidly. It is to be seen if the MTU system will be able to keep pace as the number of high-risk category patients would also increase proportionately in the coming days.
If a patient is advised home isolation, their data is supposed to go to the city’s 141 Primary Health Centres (PHCs). Each PHC is mapped to one or more wards, and PHC staff may visit the patient’s home and provide them medicines/isolation kits. According to the BBMP press release of January 18th, PHCs have distributed around 55,000 home isolation kits so far.
Hospital bed availability
According to BBMP’s COVID bed status website, the city had 6,704 government quota beds as of January 18th. Of these, around 10% beds (683) were occupied or blocked, leaving 6,021 beds available.
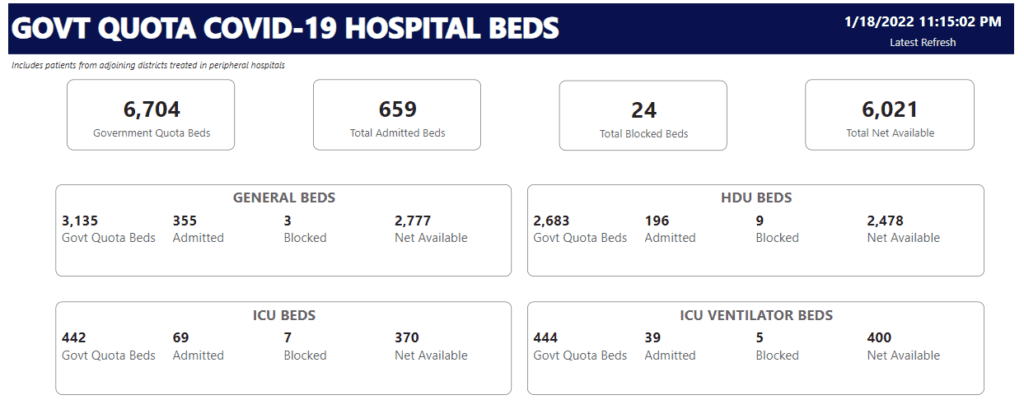
While 15% of ICU beds are currently occupied, the percentage of occupancy in other bed categories (general, HDU and ICU ventilator) is lower. The majority of beds are in private hospitals/medical colleges, but the beds allocated so far (especially in the general and HDU categories) are mostly in government hospitals/medical colleges.
As per a recent government order, private hospitals are supposed to surrender 50% of their beds for government quota COVID patients, and private medical colleges have to give up 75% of beds. “We are now focusing mainly on the bigger private hospitals that have more than 100 beds,” says Dr Bhaskar. “Most of these hospitals and private medical colleges have given beds. We don’t want smaller hospitals (those with 30, 50 beds) to have complications with respect to not having oxygen, etc.”
He says that a field team comprising senior bureaucrats as nodal officers have been verifying hospitals. “Once we have the final reports from the field that these (smaller) hospitals are fit to treat emergency cases, we will enlist those beds also. So we will have 10,000 beds in 1-2 days”.
Read more: How prepared were Mumbai’s hospitals for the third wave of COVID-19?
What about rising hospitalisation numbers
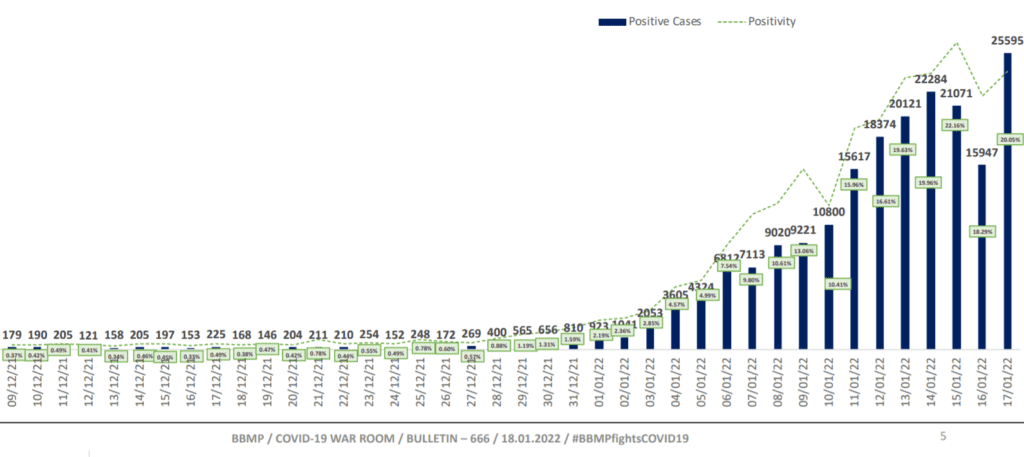
Though only 10% beds are occupied now, hospitalisations have been increasing over the past two weeks, as the graph below shows.
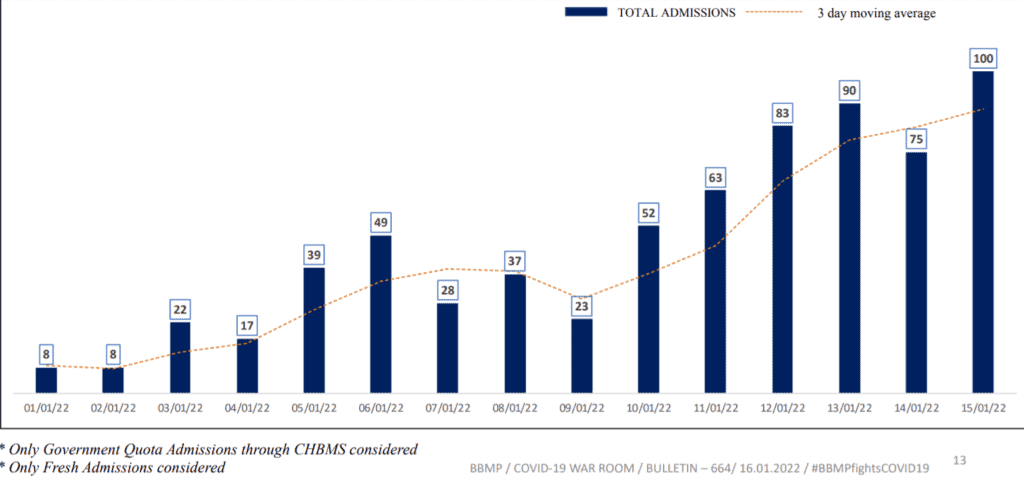
However, Dr Bhaskar says bed numbers would be sufficient, and can be scaled up if required. According to the BBMP press release of January 18th, average hospitalisation in the current wave is only 1.3%, and less than 0.5% patients are occupying critical beds.
Currently, the active caseload of the city is 1.8 lakh. “If the active caseload reaches 2.5 lakh, at 1% hospitalisation we will need only 2,500 beds,” says Dr Bhaskar. “Even if hospitalisation is needed for 10% patients then, 25,000 beds will be needed and we are prepared for it. The overall bed inventory in Bengaluru, including private hospitals, is 30,000. In that scenario, the state government might take a call on converting all those beds into COVID beds. But we are not expecting a scenario like that, we have not seen it anywhere in the world.”
Medical oxygen
Given the low rates of hospitalisation and the low oxygen requirement for patients in the current wave, Bengaluru is not facing any oxygen shortage. On January 18th, only around 300 government-quota oxygen beds (HDU/ICU/ICU ventilator) were occupied. The majority of them are stabilising patients with minimal oxygen, and the overall oxygen requirement has not been rising, says Dr Bhaskar.
“Oxygen availability is being managed at the state level. Every hospital has been mapped with their oxygen capacity, their suppliers and the type of supply they have. And the state war room has put up a central tracking mechanism which tracks the daily oxygen consumption across all hospitals, and any hospital can place a request for indenting,” he says.
Refer to this handbook by BBMP for information on COVID testing and isolation protocols, on how to avail services like hospital beds and ambulances, and for crematorium details.